Crunching the data: how’s it going?
The Australian Stroke Alliance’s comprehensive program covers a wide range of initiatives to improve urgent stroke care. We are designing and building light, portable brain scanners, and bringing together Australia’s brightest minds to improve access to urgent, pre-hospital stroke care.
We are creating sophisticated clinical and consumer education programs, led by input from rural and remote health organisations and stroke survivors. As well, data from Australia’s first digital telestroke platform and new pre-hospital air and road ambulances will help measure the health, economic, societal and commercial benefits of early treatment of strokes across Australia.
Independent analysis has forecast an economic benefit of $15.6 billion by 2050, based on the Australian Stroke Alliance’s interventions. It is essential that we assess our performance over the next five years, to ensure we are meeting targets and delivering health benefits to the nation.
National data capture for evaluation: Ourlong-term and self-sustaining policy tool will assiststate and federal health agencies beyond the 5-year horizon of the Australian Stroke Alliance program

Understanding the inequity of care
We will bring together evidence to quantify systemic historical disparities in rural, remote and Indigenous stroke outcomes. We already know that the quality of clinical care varies widely across Australia. Access to time-critical emergency treatment is often unavailable in rural or remote locations.
Data also tells us that:
- Patients in rural hospitals are less likely to receive clot-dissolving treatment for ischemic stroke
- The use of ambulance transport to hospital is 1.8 times greater if presenting to a tertiary hospital compared with regional hospitals
- Younger people (less than 65 years), those with a partner, and those with fewer comorbidities are less likely to take an ambulance to hospital.
Indigenous stroke care
The impact of stroke on Indigenous and rural communities is undeniable. For example, stroke incidence is 17 per cent higher in rural areas, particularly for Indigenous Australians where life expectancy is already 10 years shorter. According to the Australian Institute of Health and Welfare, Indigenous Australians are 1.7 times more likely to die as a result of a stroke compare with non-Indigenous Australians.
The views and expertise of Aboriginal and Torres Strait Islander people, including Elders, Traditional Owners and Native Title holders, communities and organisations are essential to overcoming the inequality experienced by Aboriginal and Torres Strait Islander people. The Alliance is committed to working with Aboriginal and Torres Strait Islander health organisations to improve the health outcomes of Indigenous communities.
Together, we will collate essential data on pre-hospital management for this patient cohort. We will build on our national data infrastructure and work with our own Rural and Remote Health Advisory Council and Indigenous Leadership Council to capture meaningful data on rural, remote and Indigenous populations.
The Australian Stroke Alliance represents a once in a lifetime opportunity to improve stroke care and outcomes for Aboriginal and Torres Strait Islander people. Supported by an Indigenous governance framework the Alliance also integrates a collaborative digital platform for stroke that supports dialogue and knowledge exchange across communities, both Indigenous and non-Indigenous.
The economic impact
The Alliance will establish a commercial benefits assessment tool, working with independent consultants, to quantify the community and economic impact of our interventions.
We will:
- Embed a health economic evaluation framework into our overall program
- Quantify clinical and societal benefits
- Identify resource savings, likely to accrue by using our novel technologies in road and air medical transportation
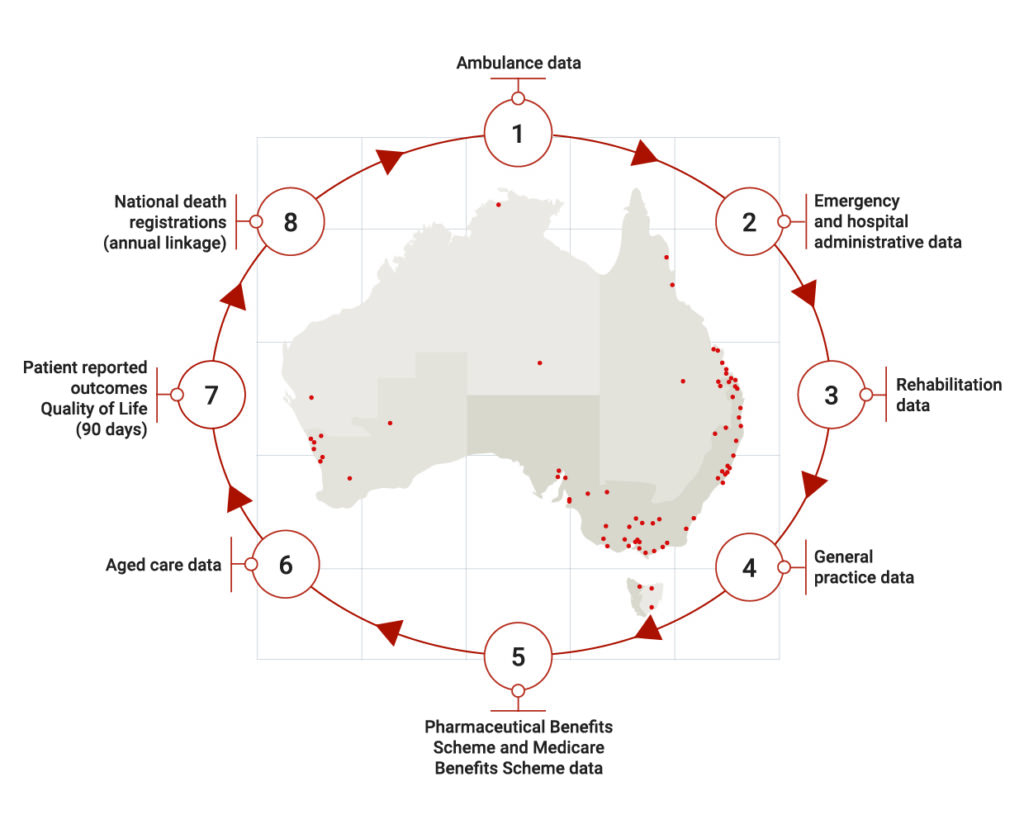
- Build continuous, systematic data collection that will link to the electronic medical record, our digital health hub and other national infrastructure platforms (see diagram above).
- Establish systems for capturing health economic metrics such as new labour (medical workers), capital (ambulances, telehealth systems), education/training (increased workforce capacity and capability) and other innovations.
Looking to the future
Our evaluation activities will identify barriers and enablers of changing systems of stroke care using surveys, interviews and focus groups, and quantitative data.
As well, we will:
- Develop optimisation models to facilitate translation of stroke research into health policy
- Build upon the Australian Stroke Data Tool, a partnership between the Stroke Foundation and Monash University, to establish new data linkages with our digital hub and national repositories (see the diagram above)
- Lay the foundation for continuous, systematic data collection to show improved equity of access for rural, remote and Indigenous populations
- Inform new government policy for pre-hospital clinical stroke services.
The great thing about the Alliance is that it is focussed on real-world issues that will be tested in the field. We’ll actively collaborate with scientists, engineers and health care workers ...and establish essential infrastructure to help us best locate these new services. (We will collect) necessary data to monitor the impact of these innovations as part of routine healthcare for stroke.
Meet Dominique Cadilhac, our Evaluation platform lead
Sign up for our newsletter to keep in-touch.