New York’s novel approach to clot retrieval
The findings of a recent trial from the United States provide more evidence for the benefits of treating stroke patients at the earliest possible timepoints while using novel strategies to provide urgent life-saving interventions.
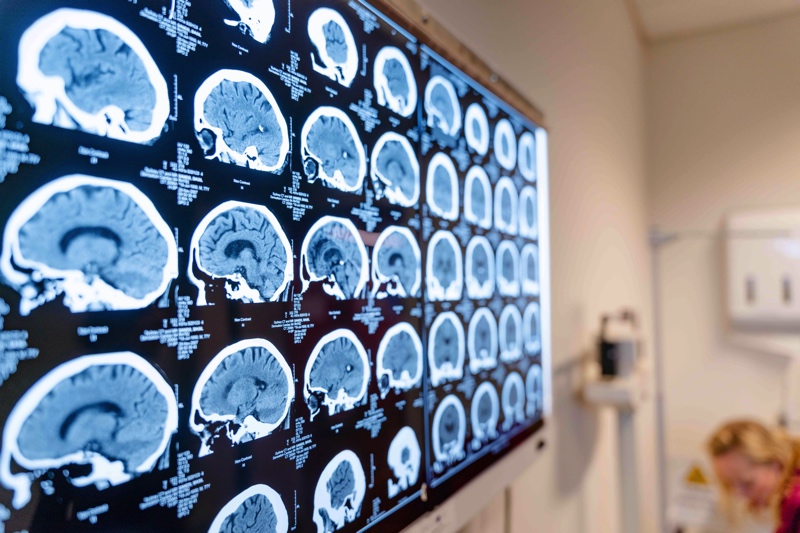
Recently, we have seen the introduction of specialised ambulances that perform stroke imaging at the scene of a patient’s stroke. These vehicles carry a team of professionals including paramedics, a radiologist, a stroke neurologist and a stroke nurse and have become known as mobile stroke units or MSUs. Having launched our first MSU in Melbourne in 2017, we have already seen it deliver impressive results which are improving outcomes for people who experience a stroke.
Last week, the results of the New York City Mobile Interventional Stroke Team (MIST) Trial from The Mount Sinai Hospital were published in the medical journal, ‘Stroke.’ Similar to the data highlighted for our local MSU, this study aimed to assess the long-term benefits of decreasing the time to treat people who experience a stroke, however, their approach was slightly different. Instead of going to the patient’s home to assess the stroke, the MIST team travel to local stroke care facilities to perform clot retrieval surgery (thrombectomy). This is an alternative approach to the current standard of care, where these patients would initially be treated with clot-busting medication (thrombolysis) at these facilities and then transferred to a comprehensive stroke care hospital for the thrombectomy surgery.
So, did the MIST strategy improve the outcomes for patients?
The answer was a quite significant yes for patients who had presented early, which was defined as less than six hours from the onset of any stroke-related symptoms. In these patients, 54 per cent had a good outcome at 90 days if they were treated using the MIST approach, as opposed to only 28 per cent of patients who underwent the standard protocol.
However, it was found that in patients who presented later (i.e. more than six hours after the onset of symptoms), there was no difference in the 90 day outcomes generated between the two strategies.
The co-chairs of the Australian Stroke Alliance, Professor Geoffrey Donnan, AO and Professor Stephen Davis, AO share their thoughts on this important work and contrast it with the key goals of our organisation:
This is an important study showing how in one US city the hospital system of thrombectomy service delivery can be modified and improved by adapting to local circumstances. It further emphasises the importance of the concept of “Time is Brain”. At the Australian Stroke Alliance, we are pushing the treatment envelope beyond the hospital into the pre-hospital environment where enormous gains in time to treatment with thrombolysis and thrombectomy can be made. We have already shown the benefits in the road based Melbourne mobile stroke unit and now plan to extend this further using ultra-lightweight imaging devices in road and air ambulances.
Different approaches to facilitation of thrombectomy have been tested in various geographical settings. There is no one size that fits all. The concept of a mobile interventional team has been shown to be effective in this study in New York City. In Melbourne, we have focussed on implementation of a validated pre-hospital score called ACT FAST to detect large vessel occlusion (LVO). This can be performed by paramedics on any ambulance and has around 80% accuracy. Our MSU allows direct diagnosis of LVO with CT angiography and then triage to an appropriate endovascular centre. We have shown that this halves the time to treatment and is cost effective.
It is fantastic to see that there is a worldwide commitment to improving the outcomes for people who experience a stroke. While different methods may be employed to achieve that goal, it remains our focus to highlight any work that extends our knowledge.